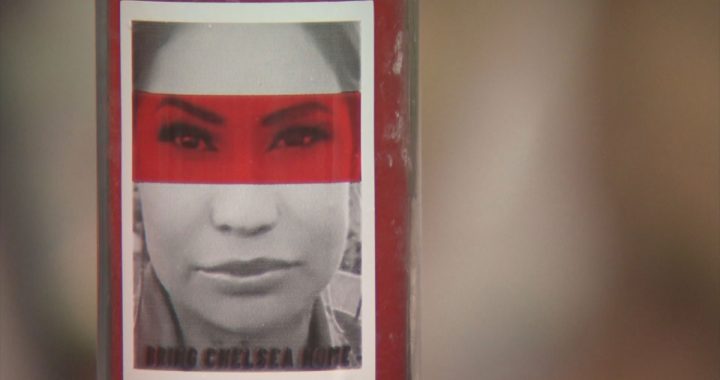
Even people who have been vaccinated are expected to “stay the course,” wearing masks and physically distancing. Photo: Odette Auger/IndigiNews
While vaccinations across British Columbia have made people more hopeful, the acting chief medical officer at First Nations Health Authority (FNHA) says it’s not time to celebrate just yet.
The first round of COVID-19 vaccines have made their way across B.C., and Dr. Shannon McDonald says her staff is feeling “more hopeful now” than they have been for many months.
“We’re definitely on the downhill of this pandemic, but there’s still so much work to do,” McDonald tells IndigiNews.
According to McDonald, 23,000 First Nations people have now been vaccinated in 120 First Nations communities across the province.
“At this stage, COVID-19 vaccines are an extra layer of protection, rather than a replacement for the public health orders and recommendations from our Provincial Health Officer, Dr. Bonnie Henry,” says a Feb. 22 post on FNHA’s website.
Staying the course
Even people who have been vaccinated are expected to “stay the course,” wearing masks and physically distancing, says McDonald.
While people may associate their vaccination with freedom, evidence shows that it takes two to three weeks for people to develop significant immunity.
“Even a vaccine that is 92 per cent or 95 per cent effective after two doses means that five to eight per cent are not protected,” she explains.
“We don’t know for sure yet, whether or not somebody who’s been immunized can still carry the virus.”
McDonald uses the example of strep throat in children, where after contracting, kids will test positive due to the bacteria, even if they’re not sick — and pass along the strep to others.
“We are concerned that even though somebody is immunized and they are protected, we don’t know for sure if they can still carry and transmit the virus to others.”
Professionals are still unsure about how well the vaccines prevent the spread of the virus, she says.
“We can’t know this until we see the impact of the vaccinations,” McDonald explains.
A small percentage of people who have been vaccinated might still be able to carry and spread the virus, she says.
Some vaccine hesitancy came from early precautions around who might not be good candidates for immune responses to vaccinations.
Good news in recent findings
While it’s still true that some people are advised against the vaccine because of preexisting health conditions, McDonald says she’s encouraged by a recent statement from the Society of Obstetricians and Gynecologists of Canada, which“very clearly [states] that the benefit of vaccine for pregnant and breastfeeding women far outweighs the risk.”
McDonald says she advises people that “if they have chronic health conditions, that may prevent them from mounting an immune response.”
She adds that she’s not talking about people with allergies, diabetes or chronic obstructive pulmonary disease.
“We really want people in those circumstances to get their [vaccines],” she says.
She says she understands there are people with vaccine hesitancy, and her recommendation is to seek out reliable information.
“It’s really important to educate yourself, and not just by Dr. Google. It’s to make sure you have trusted sources of information to help you make the decision,” she says.
FNHA offers a service called ‘Virtual Doctor of the Day,” McDonald shares, an initiative that is meant to reduce barriers for access to information and healthcare. It is intended to serve Indigenous people who have limited, or no access to their own doctors. Doctors are on call seven days a week to provide medical advice, prescriptions and referrals.
Appointments are made by calling 1.855.344.3800. A medical office assistant (MOA) will answer your call and ask for your name, Personal Health Number OR status card number, birthdate and address. The MOA will match you with an available doctor in your area, for an appointment by Zoom video call or by phone.
“There is such a gap for a lot of people in terms of having a primary care provider that they have a relationship with,” she says. The Virtual Doctor of the Day serves all Indigenous people living in B.C.
“More than half of the Virtual Doctor[s] of the Day are Indigenous physicians, which is amazing. They all have other jobs, and they do this for us to support the communities.”
McDonald says FNHA is working towards vaccinating 70 per cent of the population in B.C., which is when they can claim “community immunity,” or “herd immunity.”
But to ensure that schools, workplaces, and services remain open, people need to continue to follow health protocols, she says.
“We will still be sticking to our bubbles, staying home, only going out when absolutely necessary. No unnecessary travel and wash your hands, wash your hands, wash your hands. Wear a mask, anytime you’re in public, and especially if you’re indoors,” McDonald says.
“Those are going to be consistent messages for a while yet. I think we will all have the biggest bonfire in history to burn our masks when this is all done, but for now we still need to hang out with the mask on.”
McDonald hopes the changes in vaccine availability will bring it to more people, and earlier.
One change is the rescheduling of second doses, to be four months after the first dose, instead of one month. “The evidence now shows you’d be very well protected during that period. And then the second dose as a booster. One of the things that does is free up a whole bunch of doses, to increase the number of people that are going to get their first [dose].”
The current provincial schedule might shift to reflect an improvement in supply, expected to come in the next few weeks, says McDonald.
“That may be pushed forward depending on the supply of vaccine. We’ve had a lack of vaccine coming in for lots of different reasons, both Moderna and Pfizer vaccines have been slow to come. In the next few weeks we’re getting the normal supply and that will continue.”
McDonald also hopes the ongoing testing will result in vaccine approvals for children and youth under 18 years of age.
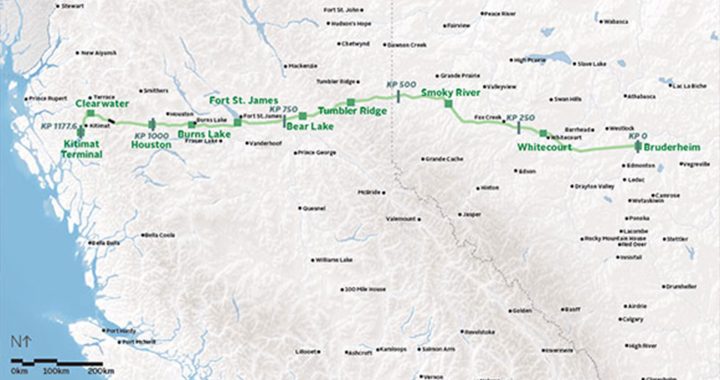
The next task for McDonald is vaccinating First Nations people who are living off reserve.
“The next piece of work that’s coming up, that I’m working with our regional teams and regional partners and the ministry, is for our urban population.”
McDonald wants “to make sure that the vaccine is going to be available to everybody.”
The larger urban mass vaccination clinics may not work for some, and McDonald is seeking vaccine clinics in places that feel culturally safe, are easily accessible, and close to transit.
“We still have a lot of work to do, but there’s a good possibility that there will be an alternative route other than just the mass vaccination planning.”
In the meantime, she has another message.
“Be kind to yourself. We’ve seen so much impact on people’s mental and spiritual health. Sometimes people will crawl into themselves and not share and not call a friend and not go out for a walk with the dog.
“Those moments of self care, of being really honest with yourself about what you’re feeling, making sure you’re getting sufficient rest, because we’re all working harder.”