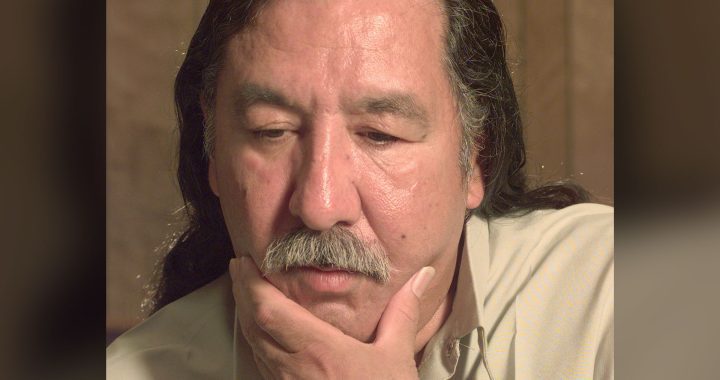
Myra Crow Chief, in an undated photo, died in an Alberta hospital in 2022.
A member of Siksika Nation in southern Alberta has launched a human rights complaint against Alberta Health Services and Strathmore District Health Services.
Ben Crow Chief claims “anti-Indigenous racism” played a role in the death of his wife, Myra Crow Chief, who was discharged from hospital on April 17, 2022, despite a test showing she had internal bleeding.
“It really hurts. I wish no one else has to go through what we went through,” Ben said at a press conference held on the Siksika Nation on Thursday. “She doesn’t get to see her kids grow up or her grandkids.”
According to the complaint filed with the Alberta Human Rights Commission, “Myra remained in the emergency department at Strathmore Hospital for the next seven hours, during which time she was persistently ignored by Hospital staff. At no point was she given a bed.
“She kept in periodic contact with Ben by cellphone during this time. Myra explained to Ben that she was trying to sleep but was unable to do so on account of the pain and nausea. She also described how she was being neglected by the nurses, who would go long stretches without checking in on her and her pain levels.”
The Alberta Human Rights Commission, which protects people from discrimination, does not confirm whether someone has filed a complaint or not.
None of the allegations in the complaint have been before the commission or tested in any court.
According to Alberta Health Services (AHS), the province is “reviewing” her case.
“These concerns are taken seriously by AHS and we are undertaking a full quality assurance review of the care provided, as well as examining the follow-up communication provided to the family,” said James Wood, director of media relations for AHS. “We offer our deepest sympathies to Mr. Crow Chief and to the family and friends of Myra Crow Chief.
“While we cannot comment on this specific case as it is before the Alberta Human Rights Commission, AHS will continue to meet with Siksika Nation to discuss their concerns.”
The complaint said Myra was rushed to Strathmore District Hospital east of Calgary in the early morning hours complaining of acute abdominal pain and waited hours for help.
“She said that no one was checking in on her or asking her about her needs,” said the complaint. “She explained how, when she was finally able to flag a nurse down, the nurse responded to her request for water briskly and with visible annoyance. Myra told Ben that, at the same time that the nurses were neglecting her, she could see them congregating and socializing among themselves.”
Later that morning, the complaint said Myra’s attending physician ordered her to be transferred to the Peter Lougheed Hospital in Calgary for a CT scan. It said after the test she arrived back at the Strathmore hospital and waited several more hours while the hospital prepared the results of the test.
“The Hospital received the scan results later that afternoon,” the complaint said. “Unbeknownst to Myra or Ben at the time, the results identified evidence of active abdominal bleeding, described in terms of a “[l]arge hematoma within the muscles of the left anterior abdominal wall … with evidence of active contrast extravasation.”
On the morning Myra fell ill and the ambulance arrived, Ben pleaded with attendants to take his wife to Foothills Hospital in Calgary instead, the complaint alleges. The ambulance attendants refused.
“Myra lived with a number of medical conditions, including chronic kidney disease, which had caused her to visit the Hospital on multiple occasions in the past,” the complaint explains. “During those visits, she and Ben had often witnessed nurses and hospital staff prioritizing non-Indigenous patients, such as by treating them first or otherwise giving them longer and more frequent attention.
“These past experiences of preferential treatment were one of the reasons why Ben had not wanted the paramedics to take his wife to Strathmore Hospital.”
The Strathmore doctor, the claim alleges, “did not inform Myra that the scan had revealed evidence [of] an active abdominal bleed. Nor was Myra provided with a copy of the CT scan results or given any prescription for pain medication. Instead, the doctor told Myra that her pain could be dealt with at her next dialysis session …”
Myra was discharged from the hospital. But, according to the complaint, her pain did not subside.
Ben ended up taking Myra to another hospital where she was diagnosed with bleeding. She died the next day “on account of abdominal bleeding.”
In the complaint, Ben wants Alberta Health to recognize the “existence of systemic racism at the Hospital and other AHS facilities and making a commitment to help end it”, conduct a comprehensive “equity audit” of the Hospital in order to identify practices and create “Indigenous roles” in the health care complaints process, and require hospital staff, including doctors, “to participate in mandatory anti-racism, cultural humility, and trauma-informed training, as developed by First Nations governing bodies and representative organizations.”
Siksika Chief Ouray Crowfoot said the Crow Chiefs’ story is one of many stories of mistreatment while receiving healthcare. In March 2022, leadership began collecting “a steady flow of complaints” from Siksika members to bring those stories to light.
This followed a January 2022 study from the University of Alberta that revealed emergency rooms across the province are treating Indigenous patients less urgently than those who are non-Indigenous.
“Far too long we’ve been subject to racism and discriminatory behaviour while receiving healthcare. For too long we’ve been insulted when we are at our most vulnerable,” Chief Crowfoot said.