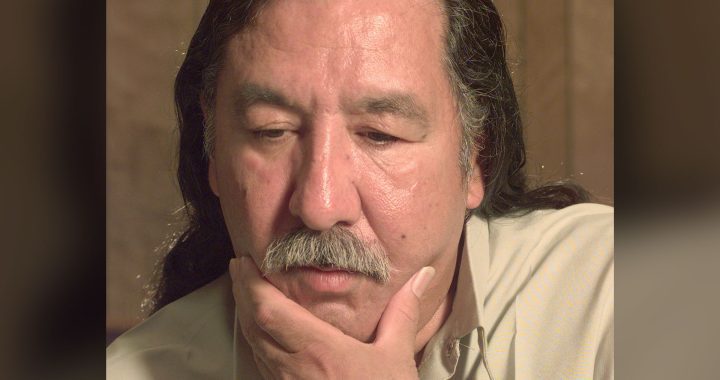
For Marion Erickson, a Dakelh woman from Nak’azdli Whut’en First Nation in north central B.C., cervical screenings – commonly known as a pap test – were just a part of life.
That was until a few years ago, when her doctor told her an abnormal pap had found precancerous cells on her cervix and that she would need a colposcopy, a minimally invasive procedure where a magnifying instrument is used to look closely at the cervix for abnormal cell changes.
Unfamiliar with the terminology or what a colposcopy would entail, Erickson says she thought the doctor was lying and that she would actually be undergoing a sterilization procedure.
“I didn’t know what that was and I always heard stories of sterilizations growing up,” she told APTN News.
Frightened, Erickson was reluctant to undergo the procedure, although she did eventually follow up.
The experience led her to write a letter to her doctor explaining why she was afraid of the procedure.
“It said ‘I thought you were going to sterilize me,’ and that was my real fear,” she tearfully recalls.
The doctor later asked Erickson if she could share part of the letter with medical students as a way to show how intergenerational trauma affects Indigenous people’s experience of the healthcare system.
The letter later led to Erickson being featured in a short video by B.C. First Nations Health Authority (FNHA) sharing her story and encouraging other Indigenous women to get screened.
“The medical community, I think they’ve tried to repair these harms,” Erickson says.
“But, there’s still instances in healthcare where we don’t trust them because we have every reason to.”
Indigenous women at risk
Cervical cancer is almost always caused by long term infection by certain types of human papillomavirus (HPV) transmitted during sexual intercourse. The government of Canada estimates more than 70 per cent of sexually active Canadian men and women will have a sexually transmitted HPV infection at some point in their lives.
According to data collected by the Canadian Cancer Society, an estimated 1,350 women were diagnosed with cervical cancer in 2020 and it’s estimated that more than 400 died from it.
Alarmingly, Indigenous women are most likely at an even greater risk of developing cervical cancer.
Dr. Sheona Mitchell-Foster, an obstetrician-gynecologist and assistant professor at University of British Columbia’s Northern Medical Program, says a 2017 study by the B.C. Cancer Agency and FNHA found a 92 per cent higher incidence of cervical cancer among First Nations women in B.C. compared to non-First Nations women.
Mitchell-Foster notes intergenerational trauma can play a part in women’s reluctance to get screened, like the forced sterilization of Indigenous women in the 1960s and 70s.
“There’s no question that if you have experienced trauma at the hands of the health care system, if generations of your family have experienced that, and when we talk about women’s health, we’re specifically talking about a very dark legacy,” she says.
“That has a huge impact, and some of those cases really weren’t that long ago.”
She adds last year’s In Plain Sight Report investigative report on B.C. healthcare delved into how Indigenous women are mistreated within the medical system.
That report found Indigenous women and girls are frequently victims of misogynistic stereotyping and disproportionately affected by poor health compared to their male counterparts.
One woman in the report recalls how a specialist manhandled her while treating her for a bladder problem. When she cried out in pain, the specialist exclaimed “Come on, you know you native women like it rough.”
“I think that you don’t need to go further than the recent In Plain Sight Report to understand why there’s this structural level racism as a barrier to care for Indigenous women,” Mitchell-Foster says.
“That’s not a new problem. This is hundreds of years in the making.”
Erickson, who works as a research manager and teaches cultural humility at UBC’s Northern Medical Program’s Health Arts Research Centre, describes medical racism against Indigenous women as “extreme conflict.
“I think of all the years of education, and that’s the attitude that comes from somebody trained in our healthcare system. This is a big problem, and so when I think about extreme conflict, you can’t get back until there’s trust built up,” she says.
“We’re never going to get past genocide until these extreme conflicts quell and we can start building trust with the Indigenous community.”
Barriers preventing screenings
Mitchell-Foster says there’s other barriers, too, preventing women from getting screened, like living far from a health care centre.
“In northern B.C. we have these vast geographies where we have to provide care to women, and depending on what season you’re travelling in, it could take several hours to get to a provider to access screenings,” she says.
A 2010 study by Western University found several barriers preventing Indigenous women from participating in cervical screenings compared to non-Indigenous women.
The study listed poverty as one barrier, as struggles with quality child care, adequate employment, and reliable transportation often affect women’s ability to get screened.
History of abuse was also noted, stating, “The majority of interviewees mentioned sexual or physical abuse as a barrier to Pap screening among some (Indigenous) women, sometimes noting that this abuse occurred in residential schools.”
One interviewee in the study states “For any woman who has experienced sexual abuse … a pelvic examination is a no-go zone, regardless of who’s doing it.”
Screenings not seen as a priority, too, was listed, stating Indigenous women often have more pressing concerns like children and elders, and that some “interviewees also noted a lack of awareness of the importance of cervical cancer screening, and knowledge about what the Pap test is.”
Comfort is key
But there is work being done to increase screenings by making the examination process less invasive.
Mitchell-Foster is leading three pilot projects in northern B.C. that provide screening kits to women and people with a cervix so they can self-screen for HPV in the comfort of their own home.
Two projects are in partnership with Carrier Sekani Family Services and FNHA in communities, respectively, in the northeast and north central interior. Those in need of a screening there can pick up kits from community health centres and self-screen at home. The results are then sent back to the centre and patients are contacted by a health care provider if they require a follow up.
The third project is in northwestern B.C. in partnership with Mètis Nation British Columbia. Similar to the other projects, patients are able to log onto a website and order a kit which is mailed to their home. The kit is then mailed back and follow up occurs if needed.
“It’s to put the tools back into their hands so they get to decide when they do the screenings and they’re able to do it themselves so they don’t have that kind of invasiveness or discomfort of requiring a pelvic examination,” Mitchell-Foster says.
So far, results have been promising.
“We’ve had really incredible uptake. Women have been so excited to be able to access this option for screenings,” she says.
Mitchell-Foster says cultural safety training is also increasing in health professions and in medical education, and that it’s part of the curriculum for medical students at UBC.
She says cultural safety training could include ensuring health care providers are fully offering continual consent to patients if they do need to have a pelvic exam, explaining why screening is being offered and what it will include, as well as letting patients know they can decline at any time.
“We’ve learned a lot about how to engage in culturally safe ways and how to include women in those decisions as well. We’re really excited about the lessons that we’ve learned and that we’re able to hopefully share on a wider scale,” she says.
Erickson, who is also a masters student at Thompson Rivers University, is working on research project to develop a Dakelh doula training program. A doula is a trained healthcare professional who provides physical, emotional and informational support to women throughout their pregnancy and birth.
She says not only will the program revitalize traditional Dakelhs midwifery practises, but also function as a way for women to feel more comfortable when accessing gynecological services.
“I think more investments in midwifery education would be a strong start to helping especially rural and remote communities because of the safety that it brings,” she says.
“It will (allow us) to take (women’s healthcare) upon ourselves as a nation together and not just one person going out of the community to be educated away from our people and away from our culture then coming back. I think it’s important to build strong foundations right in our community.”