The regional chief of the Assembly of First Nations for Ontario says First Nations leaders in the province are telling her more pandemic response money is needed immediately.
Some of the $215 million emergency funding reached remote communities Monday. It’s part of a $305 million package announced by Ottawa in March.
But RoseAnne Archibald says communities are telling her it’s not enough to re-purpose buildings or establish hospitals in First Nations.
“We need masks, we need equipment, we need cleaners, we need disinfectants. We need all the things to stop the spread and we need that money identified now,” Archibald said.
“We need it now, not tomorrow, not next week, not after breakouts are happening. Now. We need it now.”
The appeal comes as Eabametoong First Nation in northern Ontario becomes the first remote community in Ontario to confirm a positive case of COVID-19.
Located 366 km northeast of Thunder Bay, the community is one of 49 members of the Nishnawbe Aski Nation (NAN). Also known as Fort Hope, it was locked down to prevent a case from coming in.
The Sioux Lookout First Nations Health Authority (SLFNHA) says the risks posed by the virus could be amplified due to overcrowding in many First Nations.
“Now that there’s a case in the community (Fort Hope), what we are advocating for is an expanded testing strategy,” said Dr. Natalie Bocking, a family physician for the SLFNHA. “And the need I think to have a strategy that recognizes some of the challenges the remote communities face so it would need to be different than what the overall provincial strategy is because that doesn’t necessarily take into consideration the unique challenges associated with being able to quarantine or isolate in overcrowding housing.”
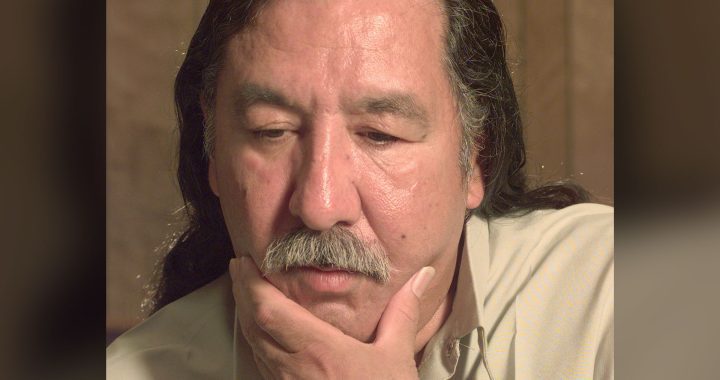
NAN Grand Chief Alvin Fiddler said the patient recently returned to Eabametoong from Thunder Bay, where COVID-19 cases have already been confirmed.
He said the man is self-isolating at home, but said the emergence of the virulent virus in Eabametoong is sounding alarms across NAN territory.
“This makes it even more real for all of us,” Fiddler said in a telephone interview from Thunder Bay. “The urgency of it all, and the importance of our communities to continue practising what we’ve been told by public health experts.”
But Fiddler said heeding that advice is more difficult in Indigenous communities than elsewhere in Canada.
The time-honoured advice to wash hands regularly, he said, will be difficult to follow in Eabametoong, which has been under a boil-water advisory since 2001.
Self-isolation, too, poses a problem in communities plagued by housing shortages and chronic over-crowding.
Fiddler said numerous NAN communities are looking into converting empty classrooms and vacant community centres into spaces where prospective patients could be kept isolated if needed.
But public health officials warned that even with preventative measures in place, the medical system serving northern communities does not have the capacity to deal with the crushing load COVID-19 has placed on other parts of Canada’s health-care apparatus.
“First Nations communities have limited access to medical facilities, medical equipment, supplies and professionals,” Bocking said. “Within all First Nation communities, there is a risk that the spread of the virus could be amplified due to overcrowding and lack of resources.”
Bocking and Fiddler both said talks are underway with various levels of government to secure key supplies, including the personal protective equipment in short supply across the province.
Premier Doug Ford said Monday the province is at risk of depleting its stock of masks, gowns, gloves and other gear within a week without a renewal of supplies from the United States.
Canada’s top doctor, meanwhile, acknowledged the public health advice guiding the rest of the country can’t be applied in the same way across Canada’s Indigenous communities.
“We’ve issued guidance for public health actions in more remote and rural settings as well, and those do have to be adapted to the realities of what’s on the ground,” Dr. Theresa Tam told a Monday news conference without providing specific details of how guidelines have been revised.
Fiddler said remote communities are increasingly concerned about the potential spread of COVID-19, which has surfaced in a number of cities that serve as key gateways to more remote first nations. He said those include northern urban centres such as Timmins, Sioux Lookout and Dryden.
The sorts of physical distancing measures that have transformed daily life across much of the country, he said, have taken hold in more remote areas over the past week-and-a-half.
“There’s a growing sense that this is a real threat to our communities,” he said. “We have to do everything we can to try and prevent it.”
Financial aid package application opens
The federal government opened the window on a portion of the $305 million aid package aimed at helping First Nation, Metis and Inuit people and businesses through the COVID-19 pandemic.
The money, announced March 18, is part of a larger $82 billion dollar package that Canada is hoping will help people who have been put out of work and businesses that have had to close shop to prevent the spread of the novel coronavirus that has to date, killed nearly 70,000 people worldwide.
Two hundred and eighty deaths are being reported in Canada of this posting.
At the moment, $15 million will be available Monday for urban and off-reserve Indigenous organizations through the Indigenous Community Support Fund.
According to the government, all national, regional and local Indigenous service delivery organizations supporting Indigenous peoples living in urban centres, off-reserve organizations supporting their members living away from their communities, other Indigenous organizations or communities providing services to people living off reserve in urban centres and are not eligible for money from other programs.
The deadline to apply is April 13.
Non medical masks can keep people with COVID-19 from spreading it
Tam said Monday that wearing a mask is a way for someone who might have COVID-19 without realizing to keep from spreading the illness to others.
That’s a change from previous advice.
Tam says the shift is due to increasing evidence that people with the virus can spread it without knowing they’re sick.
She says masks worn this way protect others more than they protect the people wearing them, and don’t exempt wearers from all the other measures they should take against COVID-19, including physical distancing and regular handwashing.
And Tam says medical masks still need to be preserved for front-line health workers, so cloth masks and other alternatives are the way to go.
She says a non-medical mask can reduce the chance of respiratory droplets coming into contact with others – for instance, on a bus or in a grocery store.
With files from Willow Fiddler, Allana McDougall and The Canadian Press