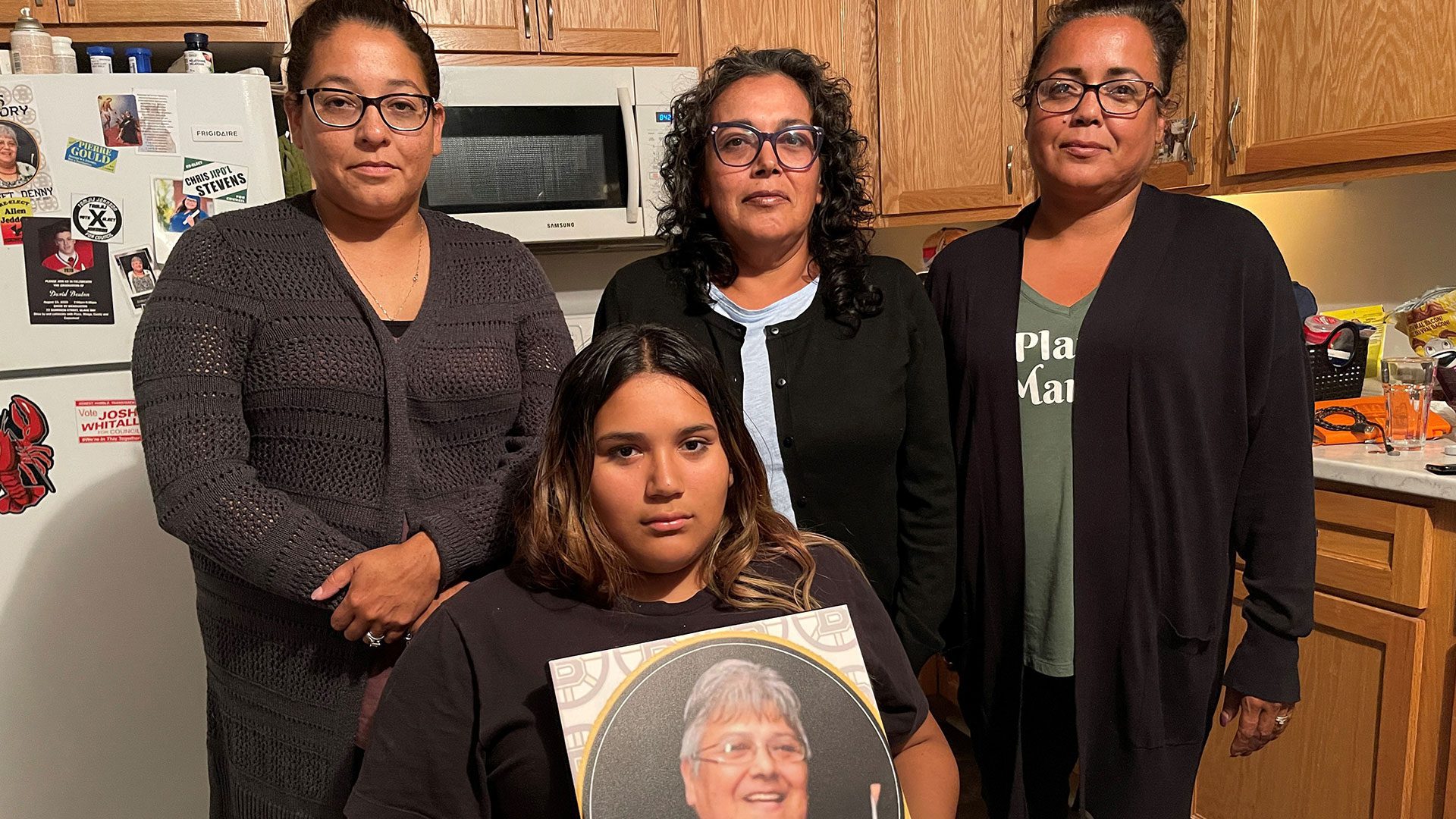
Lynn Francis is looking for answers after her mother, Bridget Anne Denny, 65, died while in care at the regional hospital in Cape Breton.
“I thought she had the care she needed when we left her that evening, so I was really in shock,” said Lynn Francis.
Bridget Anne Denny, 65, died unexpectedly while in care at the Cape Breton Regional Hospital on Jan. 20, 2021.
Denny, a residential school survivor, mother of five, grandmother to 15, Mi’kmaw language speaker, and an active member of her community, the Eskasoni First Nation, went to the hospital on Jan. 19, 2021, for pain and complications from her diabetes.
MaryI Joe-Francis, Bridget’s daughter-in-law, said she died the next morning and the doctor on shift said an autopsy wasn’t necessary.
“She advised that an autopsy wasn’t really needed because she had so many health issues but really, we didn’t have, we didn’t know how she died,” said Joe-Francis.
Denny’s body was cremated and days before the funeral, the family found out from another patient that Denny had fallen in the middle of the night.
“That was not brought up when we had the conversation with the doctor and the nurses, we were there for hours after she had passed away, the whole family was there,” said Joe-Francis.
Joe-Francis obtained Denny’s medical chart, then filed a complaint with the Nova Scotia College of Physicians and Surgeons of Nova Scotia.
“If we had known she had fallen, that all that stuff was wrong with her the night before, we would have wanted an autopsy. The medical examiner wasn’t even made aware of her death because it was just kind of like brushed off,” said Joe-Francis.
Joe-Francis met with hospital staff for answers, with no success.
“I would say it’s heated actually like it was a lot of back and forth but a lot of anger and frustrations from us, we wanted answers and we didn’t get any, we left there even angrier than we were that day because they had nothing, they had nothing,” said Joe-Francis.
The incident sparked an investigation under the Protection for Persons in Care Act.
A final report issued on Feb. 25, 2021 concluded:
“The facility failed to provide adequate care based on the lack of documentation … in response to the affected patient’s unwitnessed fall, including failing to document the affected patient’s post fall vitals and post fall assessments firsthand, staff inaccurately completed the affected patient’s admission fall risk assessment and hourly checks, and no documented evidence that post fall neuro vitals and a SIMS report were completed.”
The report also said, “it is beyond the scope of this investigation to determine if this contributed to the affected patient’s death.”
Associate professor of ethics at Dalhousie University Lynette Reid, can’t comment directly on Denny’s case, but said inadequate care is unethical.
“When unsafe care is being delivered then a line is being crossed,” said Reid.
According to the report, even staff were shocked by Denny’s death stating: “All staff interviewed reported they were “surprised” and “shocked” by the death of the affected patient.”
One staff reported the death of the affected patient as “unexpected.”
The report requested the hospital’s policy on unexpected death, including the process to notify the medical examiner, but the hospital would not provide the policy.
According to the report, had the doctor known about the fall, the medical examiner would have been notified.
Francis said she was devastated by this information.
She and the family went through a time of mourning – and trying to figure out what to do next about the situation before coming to APTN News.
“I was disgusted with the report, I can’t believe they are actually treating patients like that especially when your Native they brush you off,” said Francis.
The report said Denny’s fall injury risk assessment was inaccurate.
“As evidenced by incorrect scoring for two identified risks, ie: IV and history of falls, it did not include the date, time and signature of the person who completed the assessment,” said the report. “This inaccurate assessment resulted in the affected patient being identified as a low risk for falls, and therefore, the additional high risk for falls interventions were not considered.”
Joe-Francis wonders if discrimination had a factor in Denny’s death, and hopes to find answers.
Part 2 of this story is coming.