The Canadian Press
First Nations leaders in British Columbia say they suspect the deadly opioid fentanyl is having a disproportionate impact on their communities but they can’t get the numbers to prove it.
Grand Chief Edward John of the First Nations Summit said he’s been asking the First Nations Health Authority and other provincial authorities for the data since last fall but nothing has yet been delivered.
“I don’t even know how to feel, we need to have that information and we shouldn’t wait to act,” he said.
Over 900 people died in the province from illicit overdoses last year. John said although he doesn’t know what proportion of those who died are Indigenous, he knows plenty of families and communities that have fallen victim to the crisis.
“All I hear is the anecdotal information from communities where funerals are taking place,” he said “People are dying needlessly.”
The First Nations Health Authority said it’s working with the BC Coroners Service to develop an approach to collect the data that would identify deceased individuals as Aboriginal.
Current data collected by the agencies is based on self-identification and must first be compared against the B.C. Ministry of Health’s First Nation client file, which includes data from the federal government.
“We want to ensure that any publicly released Aboriginal specific data is as accurate as possible,” said Dr. Shannon McDonald, deputy chief medical officer for the First Nations Health Authority, in an email statement.
“Once the data matching is completed and there’s greater confidence in the numbers, it will be available for release,” she said, adding that numbers may not be available for a few weeks at least.
In the meantime, the health authority said it’s addressing the overdose crisis by educating the public about the harmful potential of opioids and distributing naloxone, the overdose-reversing drug.
More than 70 First Nations health centres have received naloxone kits and the health authority said it held over 110 public training sessions on how to use the kits last year.
Despite these efforts to get ahead of the crisis, the Shuswap Nation Tribal Council declared a state of emergency after seeing too many deaths in its communities. The council represents a collection of First Nations bands in the B.C. Interior.
Tribal Chief Wayne Christian said in the days leading up to the declaration in March, five band members were buried in the span of a week.
“Any death is an emergency,” he said. “The grief and loss, compounded by the intergenerational trauma, people just said we have got to do something about this, enough is enough.”
Christian said the council is using the declaration to draw attention to the issue and educate people of all ages about addictions and drug use.
More people seem to be aware of the crisis now, he said, but the history of residential schools and abuse still leave many vulnerable to addiction and other health issues.
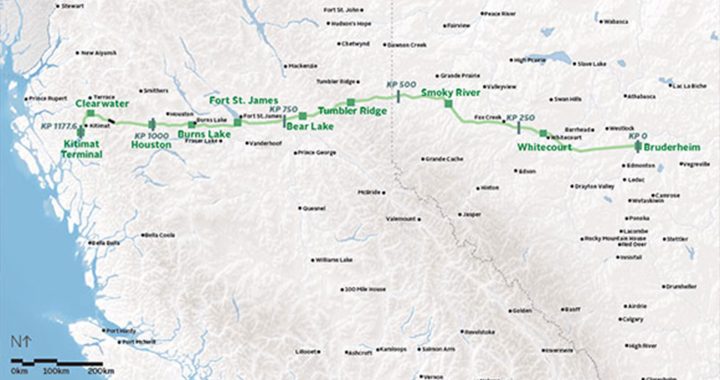
Terry Teegee, tribal chief of the Carrier Sekani Tribal Council, said another problem rural and remote communities face is the proximity to health care services.
He said the closest doctors for his people in the Takla Lake community are in Fort Saint James in north-central B.C., which he added is an area struggling to recruit and keep physicians. His people travel 5 1/2 hours to reach Prince George if they need a specialist, he said, or at times have to go even farther to Kamloops or Vancouver.
“Just the distance is, I suppose, you could define it as a health detriment in terms of accessing proper health care,” Teegee said.
There are 10 treatment programs with a total of 239 beds available to Indigenous people in B.C. through the health authority, including one youth program. The health authority said some programs offer immediate treatment while others have a 10 to 12-week waiting list.
If there is a shortfall for services, John said overdose data could help First Nations leaders advocate for better resources when it comes to health care and addictions treatment.
Christian, who has worked with one of the addiction treatment programs, said even without data, there are many areas where health care can improve. He said there is a need for post-treatment services that prevent people from relapsing and for programs addressing the trauma that leads to addictions.
“Addictions is a system. The person comes out of a family, and yeah you can treat the one individual, but it’s the whole family system that needs to be treated,” he said.
Any data released can’t represent the effect overdose deaths are having on communities, he said.
“The hard part for me, when people talk statistics … those numbers aren’t numbers to us, those are our relatives,” Christian said.