Atikamekw leaders are renewing their calls for the Quebec government to recognize systemic racism in the province’s health-care system.
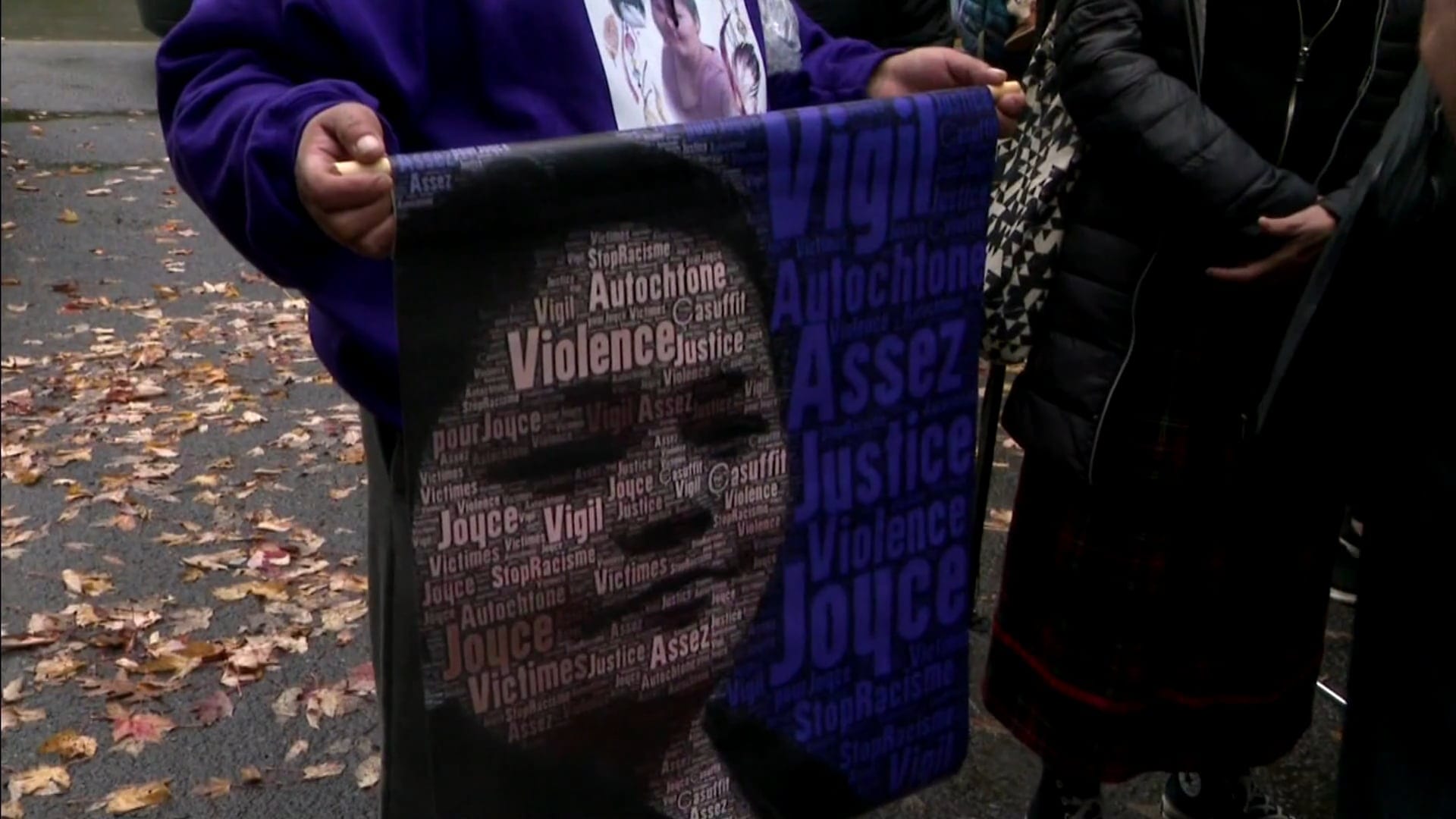
Paul-Emile Ottawa, chief of the Atikamekw Council of Manawan, testified Tuesday at the coroner’s inquest into the death of Joyce Echaquan and said her passing has left an open wound in the community, located about 250 kilometres north of Montreal.
“All we’re asking for is the right to live in dignity,” Ottawa told reporters outside the Trois-Rivieres courtroom.
“Quebec society is still debating our right to die with dignity. These are discussions we’re still having now.”
Chief Ottawa’s recommendations include having doctors and other health-care staff trained in school on the realities of the country’s Indigenous Peoples, simplifying the hospital complaints process, and recognizing systemic racism.
Echaquan, a 37-year-old Atikamekw mother of seven, filmed herself on Facebook Live as a nurse and an orderly were heard making derogatory comments shortly before her death last September at a hospital northeast of Montreal.
Constant Awashish, grand chief of the Conseil de la Nation Atikamekw, told the inquiry Tuesday that Quebec Premier Francois Legault should reflect carefully on the issue of systemic racism instead of denying it exists.
“That’s what it is – ‘Joyce’s Principle,’” Awashish explained. “I think we need to give Canadians and Quebecers better education and better awareness on First Nations.
“And yes, there’s the word ‘systemic racism’ in [‘Joyce’s Principle’] – but I think if we open our eyes, systemic racism isn’t only the Indian Act. It’s way beyond that.”
Reform needed to reduce Indigenous patients’ fear of health system

Innu surgeon Dr. Stanley Vollant testified on Monday that Indigenous patients are afraid of seeking care due to systemic racism and the poor treatment they encounter in Quebec’s health network.
Vollant said Echaquan’s death reinforced the feelings of insecurity among Indigenous patients. He said he believes systemic racism is entrenched in the health system and worries Echaquan’s case will not be the last of its kind.
“There will be others, I’m certain; we still deny the evidence,” Vollant said.
As the inquiry began its recommendations phase on Monday, Vollant urged the provincial government to introduce cultural security policies to reduce fear among Indigenous patients seeking treatment in Quebec hospitals.
Vollant said cultural security – a concept that ensures health care is provided with respect for a patient’s cultural identity – is vital. The concept originated in New Zealand in the 1990s, where the Maori population lacked confidence in that country’s health network.
He recommended creating multidisciplinary teams, including community liaison officers, to help Indigenous patients navigate the health-care system.
Vollant said the liaison officers need to feel supported by hospitals and the provincial government. The Echaquan inquiry has heard the Joliette hospital had an Atikamekw liaison officer who was ignored and underused and had quit the job.
The complaints process should be simplified because it isn’t in the nature of Indigenous patients to file official grievances, Vollant said.
Professional orders, he added, need to better educate their members about First Nations communities and forbid discriminatory behaviour. Respect could be as simple as saying hello in the patient’s mother tongue, Vollant said.
Last November, the Quebec government announced a $15-million investment to improve cultural security among First Nations and Inuit communities by hiring liaison officers as well as Indigenous employees to serve as guides for patients navigating the health-care network. A Health Department official testified Monday the cultural safety plan is a government priority.
Vollant offered his own mea culpa, recounting that in 2012, he was skeptical when he met Atikamekw community members who voiced their concerns about the Joliette hospital. “I’m a doctor, so I’m part of the medical establishment. I listened to these stories with a doubt, thinking maybe they had misunderstood, there was a cultural difference, that it was poorly interpreted,” Vollant said.
“Systemic racism is invisible, we don’t see it,” he added. “Even an Indigenous person can become white inside. The culture that we’re taught, the education that I received, is that of the majority, the colonial system.”
Dr. Jacques Ramsay, who is assisting coroner Gehane Kamel in the inquiry, asked whether there was a way around the term “systemic racism,” which has been controversial in Quebec and has led to denials from Premier Francois Legault and his ministers.
“I know the term systemic racism gives hives to many people, and maybe it’s obstructing in improving health care for First Nations,” Vollant replied. “As I’ve said, if someone isn’t able to name the elephant in the room here, if they call it a ‘pachyderm with big ears’ but find solutions to the problem, I’m in favour.”
Vollant said there isn’t any need for more commissions, just action, noting the impact of the inequality is well documented in studies that found that First Nations patients are at an increased risk of complications or death because they wait too long to seek diagnosis.
Dr. Samir Shaheen-Hussain, a Montreal pediatric emergency room physician who has written about medical colonialism and fought against a Quebec policy that forbade parents from accompanying sick kids on emergency air evacuations, said in his estimation, Echaquan wasn’t “ignored” but rather “despised to death.”
Hussain recommended that the Quebec government adopt ‘Joyce’s Principle,’ a set of measures aimed at ensuring equitable access to health care for Indigenous patients, adopted by the community after Echaquan’s death.
That principle, however, has not been taken up by the government because of its reference to systemic racism.
“In the end, it’s medical colonialism that is the cause of death of Joyce Echaquan and as a society, we all have a responsibility to ensure such an inevitable death doesn’t happen again,” Hussain said.
For her part, during her testimony, Viviane Michel, President of Quebec Native Women, issued several recommendations centering on “training and internal laws to counter racism, discrimination [and] prejudices” while increasing accountability.
“Say, for example, someone witnesses or overhears racial or dehumanizing remarks towards an Indigenous patient – we have to have mechanisms to protect these people who want to denounce,” Michel explained.
“We talk a lot about an Indigenous ombudsman, and we need to include First Nations in all of these processes,” Michel added. “Especially the complaint process, so victims are accompanied and sent in the right direction, and so there’s a follow-up for these complaints.”
The Quebec coroner’s role is to examine the circumstances of Echaquan’s death and issue recommendations on how to prevent them from happening again.
The inquiry is scheduled to end on Wednesday.
With files from the Canadian Press