Heather Winterstein died in 2022 after two trips to the St. Catherines Hospital.
A report detailing the grueling final days of Heather Winterstein’s life says some staff are “fearful” of treating Indigenous patients because they are unsure of the cultural correctness needed.
“The Panel heard that ED [emergency department] staff are now fearful of treating/interacting with Indigenous patients as they do not know what to do differently from what they have done in the past or do currently,” said the report.
The report, released Aug. 28, is the work of a panel put together by the Niagara Health in response to Winterstein’s death.
The 24-year-old, whose mother is from Six Nations of the Grand River, died of a staph infection after two visits to the St. Catharines Hospital – located near Niagara Falls, Ont.
Both times Winterstein was taken to the hospital it was in an ambulance for acute pain.
The first time, she was given pain medication and “despite abnormal vital signs at triage, discharged her without a reassessment of the vital signs.” The discharge diagnosis was documented as “social issues.”
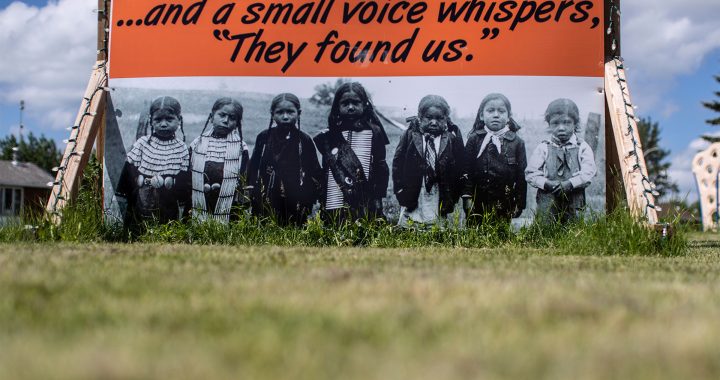
“Heather manifested some of the most acute symptoms of Indigenous health inequities,” the report says. “She was marginalized, underhoused, and living in poverty. She arrived on both visits by ambulance. The paramedic assessment and documentation for both visits may have introduced an unconscious bias that impacted Heather’s care.”
Winterstein was given a bus ticket and sent home on a 90-minute trip.
Read More:
Six Nations mother looking to create ‘Heather’s Law’ after daughter’s death
On Dec. 9, 2021, on her second trip to the emergency room, she was moved from a stretcher to a wheelchair where she spent two and a half hours waiting to be brought into the “Rapid Assessment Zone.”
The panel was able to access video inside the emergency department on the night.
“The Panel reviewed the video file footage of her time spent in the waiting room. It was difficult to witness,” the panel reported. “Heather is seen in a wheelchair where she is restless and appears to be unable to find a comfortable position. She is seen lying on the waiting room floor again, restless and unsettled.
“On several occasions, staff from housekeeping and security are seen getting her a blanket and assisting her back into a wheelchair. Another patient in the ED waiting room is seen assisting her by pushing her wheelchair to the triage desk to speak to the nurse.”
Not long after, Winterstein is seen on the video collapsing in the waiting room again. She’s eventually transferred onto a stretcher and taken to the Critical Care Unit. She died shortly after. According to the panel report, the family was “only notified after she was transferred to the Critical Care Unit.”
When her extended family arrived at the hospital, “all information about Heather was provided by the spiritual staff versus the clinical staff and this felt dismissive.”
Staff at the hospital

According to the report, doctors and emergency room staff were “reluctant” to speak to the panel about Winterstein’s death. The frontline staff who did connect with the panel “describe themselves as dedicated,” but some noted that some nurses in the emergency room “lack empathy and compassion.”
They were defensive about accusations of Winterstein’s care “being impacted by racism or bias.” According to the report, several “expressed the sentiment that Indigenous culture training was imposed on them.”
Recommendations
The panel issued ten recommendations to the Niagara Health Authority including the need for them to “allocate time, resources and energy to instill cultural safety throughout the organization’s staff, physicians and volunteers.” Other recommendations are directing the health authority to be open to learning from and about others, championing cultural sensitivity, respecting cultural differences, and educating people about assumptions people make about people.
- The path to cultural safety includes the following steps (as adapted from the work of the Northern Health Indigenous Health): Committed leadership is required to champion change throughout the organization and to ensure that change is sustained. Cultural humility is a building block for cultural safety.
- Niagara Health should continue to collaborate with the Indigenous community to promote a safe and welcoming environment at all current and future sites. As an example of work recently initiated, Niagara Health unveiled Indigenous artwork at the St. Catharines Hospital, and the plan for an Indigenous Healing Centre, at the new South Niagara hospital.
- Niagara Health should promote the Indigenous Patient Navigator Team to patients, families, and the community, as well as to all staff, volunteers, and physicians. Information should be made available at all patient/family entrances and access points at all Niagara Health sites.
- Niagara Health should seek out Indigenous representation for the governance and decision making bodies, and on any advisory councils to ensure a focus on Indigenous care.
- The Niagara Health Quality Improvement and Strategic Operating Plans should reflect the need for relationship building and ongoing engagement with the Indigenous community.
- Niagara Health should work with Indigenous communities on the recruitment and retention of Indigenous employees, physicians and volunteers.
- Niagara Health should develop strategies to focus on the health and well-being of Emergency Department and hospital staff to allow them to continue to provide compassionate care.
- Niagara Health should develop clear expectations and accountability for staff, volunteers, and physicians throughout the organization to ensure success in providing culturally safe care.
- Niagara Health should, in Heather’s memory, host an annual gathering, with the community, to provide updates on the implementation and progress of the recommendations received from the internal and external reviews and this report. This annual gathering could be initiated in 2023 with a Healing Ceremony.